EMS1 Article – Order from chaos, meaning from numbers: The EMS data reset
Dr. Ed Racht calls for healthcare-first framing, action-oriented dashboards and the courage to celebrate wins — and be horrified by failures
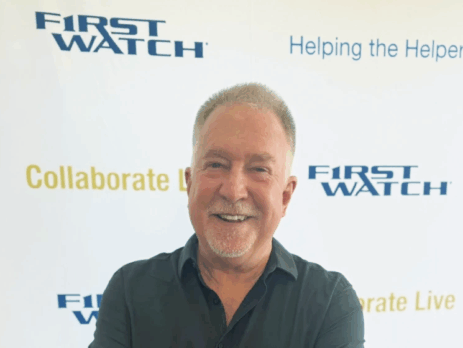
At this year’s FirstWatch Collaborate Live conference, Dr. Ed Racht, chief medical officer for Global Medical Response (GMR), took the stage with trademark humor, humility and a challenge that hit home for every EMS professional in the room: it’s time to stop treating data as cold, lifeless numbers.
“I love to create order from chaos,” Dr. Racht began. “That’s what we all do.” But, he added, the same love of order that drives EMS clinicians to make sense of complex, high-stakes scenes must now be applied to the ever-growing universe of EMS data. Numbers, charts and dashboards only take us so far. Facts may be science, but without emotion, they rarely inspire action.
The science and the spark
Dr. Racht reminded the audience that science is non-negotiable: “The nice thing about science is that it’s true whether or not you believe it.” Yet, he argued, that data must be infused with story and meaning. “It’s time to make facts emotional,” he said, urging leaders to connect performance metrics to patient outcomes, community expectations and crew pride.
He compared EMS data use to the way Spotify recommends songs or Waze reroutes drivers. Those tools take raw information and translate it into something personal, actionable and, most importantly, human. EMS, he said, can and should do the same. “Data should not just tell us what happened; it should move us to do something about it.”
Healthcare, not transport
Dr. Racht also pushed back against the long-standing tendency to define EMS as medical transportation. “Our product isn’t a ride,” he said. “Our product is healthcare and peace of mind.” Every dispatch, every metric and every improvement initiative should reflect that truth.
He illustrated the point with vivid frontline examples: the shift from managing penetrating trauma to mass-casualty blunt trauma, the evolution of triage systems, and the emotional complexity of policies like limiting lights and sirens use. Science, he noted, can guide decisions — but emotion determines whether those decisions stick.
Making data feel human
In one moment, Dr. Racht turned from humor to heart. “If a city’s neurologically intact cardiac arrest survival rate is zero, that’s data,” he said. “But it should horrify us. Because if that’s my mom, that’s not a statistic; it’s a tragedy.”
That emotional response, he argued, is precisely what must drive improvement. Leaders should celebrate progress, confront failure and make room for both passion and discomfort in their data discussions. “When you care, you act,” he said. “And when you act, you change lives.”
From dashboards to decisions
Dr. Racht’s keynote was less about analytics and more about culture. He challenged attendees to create systems that don’t just report numbers but recommend actions — tools that help field crews, managers and policymakers make better, faster, more compassionate decisions.
As Dr. Racht always does, he drew the audience in with his inimitable humor, using it to craft vivid points, but the through-line was serious: EMS is a healthcare profession built on trust, science and emotion in equal measure.
As Dr. Racht closed, he left the audience with a simple challenge: “Get emotional about your data. Celebrate the wins. Be horrified where you need to be. Then do something about it.”
Dr. Racht’s message resonates far beyond the conference hall. In a field defined by speed, complexity and compassion, data is only powerful when it connects to the human experience it represents. In EMS, emotion isn’t the enemy of science, it’s the force that turns science into care.
Key messages
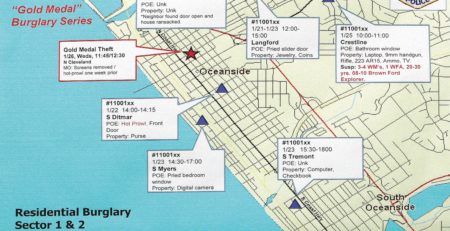
Order from chaos is the EMS superpower. We operate with little time, partial data, and big consequences—so our information must be instantly useful.
Facts – story – action. Data are objective; leaders must make facts emotional so stakeholders feel urgency and accountability.
Science is non-negotiable. Use evidence as “true north,” then pair it with narrative to change policy and practice (e.g., L&S use).
Our product is healthcare (and reassurance), not rides. Frame metrics and investments accordingly.
Borrow from consumer tech. Personalize, predict, and simplify—don’t just report numbers, recommend actions.
MCI and triage realities. Traditional tools can fail at scale; learn from events.
Celebrate and confront. Publicly recognize improvement; be candid where outcomes are unacceptable to catalyze change.
Continuous curiosity. Keep asking, “Is there a better way?”—from cardiac arrest medications to alternative destinations and care pathways.
Practical takeaways for EMS leaders
Wrap metrics in meaning. Pair every KPI with a patient story, a visual, and a concrete next step.
Design for decision-making. Present data the way Waze does: “Turn here”—i.e., policy recommendations, checklists, and playbooks.
Align language with mission. Replace “transport” framing with healthcare and outcomes in reports, briefings, and funding asks.
Show your work—visibly. Post station-level performance, celebrate high performers, and support those who need improvement.
Pilot, measure, adjust. Treat protocol changes (e.g., sirens, arrest bundles) as tests with predetermined success metrics.
Plan for the new MCIs. Update triage, comms, and hospital distribution strategies for both penetrating and blunt, high-volume events.
Leverage AI carefully. Use it to route resources, prioritize patients, and forecast demand—always anchored in validated science.
Originally printed in EMS1 and reproduced here with the permission of the author, Rob Lawrence. View Article