Measles (Rubeola) Update
IN THE NEWS
Finally, after a year, almost all the news about measles is good. Case numbers were way down in September compared to previous months, the outbreaks in New York City and State, which provided three-quarters of all the cases in 2018 and 2019, were declared over just days shy of their one-year anniversary and, because of that, the United States will likely maintain their WHO Measles Elimination status of 19 years. Unfortunately, a new outbreak in New York State has begun, identified as New York State #2. An outbreak is defined as three (3) or more linked cases.
According to the CDC, from January 1 through October 3, 2019, there have been 1250 confirmed cases of measles in 31 states; 75% of them were in or linked to New York. Although seven (7) new cases were added in the last week, only three (3) were new cases; the remaining four (4) were attributed to previous weeks. Measles can and do cause serious complications. Of the total cases in 2019, there were 119 who had to be hospitalized and 61 had serious complications such as encephalitis and pneumonia. That’s a hospitalization rate of 9.5%. Note: previously reported hospitalization and complication numbers have been adjusted downwards. There have been no reported deaths.
The following 31 states have reported measles cases to CDC in 2019:
Alaska, Arizona, California, Colorado, Connecticut, Florida, Georgia, Idaho, Illinois, Indiana, Iowa, Kentucky, Maine, Maryland, Massachusetts, Michigan, Missouri, New Mexico, Nevada, New Hampshire, New Jersey, New York, Oklahoma, Oregon, Pennsylvania, Texas, Tennessee, Virginia, & Washington.
Note: bold indicates an outbreak state; non-bold represents states with individual cases or previous outbreak(s) that are now controlled.
This is the largest number of cases tallied in the past 27 years (1992); eight (8) years before measles was considered eradicated from the U.S (2002). In fact, these cases were largely within pockets of socially close groups of unvaccinated individuals. The outbreaks were initially linked to imported cases from countries that had large measles outbreaks such as Israel, Ukraine, and the Philippines and then spread to those in the community who were unvaccinated or undervaccinated. Imported cases occur when U.S. residents travel to other countries and are infected or infected individuals from other countries visit the U.S. This travel usually occurs during the incubation period when symptoms of measles are not yet apparent. There are many areas around the world where measles is still common and often more deadly.
Measles Cases Reported by Month in 2019*
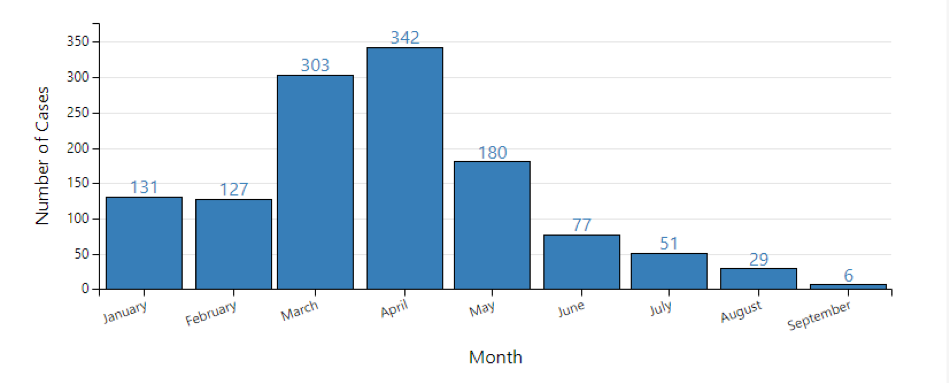
*Reporting for 2019 began December 30, 2018. Case count is preliminary and subject to change.
Number of Measles Cases Reported by Year 2010-2019 **(as of October 3, 2019)
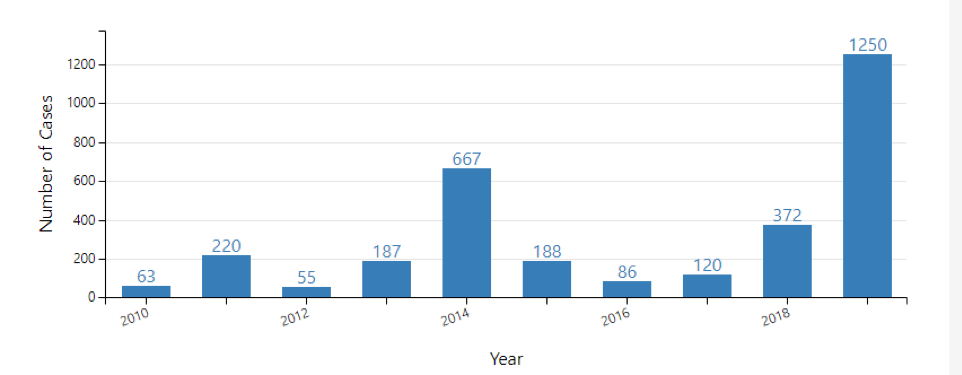
**Cases as of October 3, 2019. Case count is preliminary & subject to change.
Data are updated every Monday.
Both Charts were copied from the CDC Website: Measles Cases and Outbreaks @
https://www.cdc.gov/measles/cases-outbreaks.html; page last reviewed: October 7, 2019; Accessed 10-8-19.
Typically, if an imported case is brought to a community with a high vaccination rate, an outbreak does not occur or is small and quickly contained. This is why vaccination against measles is so important since travelers will likely continue to bring measles into the U.S. Only high levels of vaccination rates, early identification & diagnosis of measles, as well as surveillance & control measures will limit the spread of measles amongst individuals and communities in the United States.
There are individuals that cannot be vaccinated due to valid medical reasons or who are otherwise immunocompromised and at risk for contracting measles and other vaccine-preventable infectious diseases if exposed. And, because of their immunocompromised state, these infectious diseases can be lethal. Herd immunity protects these individuals. Since they cannot be vaccinated or their immune systems will not retain the immunity, they rely on those in the community who can be and are vaccinated, to surround them with immunity so that measles and other vaccine-preventable illnesses don’t reach them. It must be noted that there is a difference between those that are not medically eligible for vaccination (too young or otherwise not able to be vaccinated due to allergy or some type of immunocompromise) and those that have philosophical reasons not to vaccinate. Some states, counties or outbreak areas have blocked all but validated medical exemptions from being honored, although different approaches have differed have been used.
During an ongoing outbreak, the CDC/ACIP (Advisory Committee on Immunization Practices) may recommend infants between 6-11 months receive one (1) dose of MMR who live in or are traveling to areas in the U.S. where there is ongoing measles transmission occurring in that community. A second dose of MMR may also be recommended for those 1– 4 years old and/or adults who have had only one dose of MMR previously, depending on what age group(s) are affected in the community. Local health departments will have this information, and post it, if any of these recommendations are in place.
The CDC/ACIP standard recommendation for those 12 months through adulthood, and traveling internationally, is vaccination with two doses of MMR following the routine immunization schedule, with all being fully vaccinated before travel. Infants 6-11 months should receive one (1) dose of MMR prior to travel but this does NOT count as the first dose in their routine MMR vaccination schedule. Pediatricians, local health departments, and travel medicine clinics will be familiar with these recommendations and provide appropriate vaccination care.
As mentioned above, the WHO has Measles Elimination program, and the U.S. has had the designation as a country with measles eliminated since 2000. The ongoing measles outbreaks that began in New City and State in 2018 put that status at risk, since an outbreak in a specific geographic area that goes on for more than a year suggests that a disease is becoming part of the community (endemic) and not just a group of cases related to imported cases from travel. Although the U.S.’s measles surveillance and data will be reviewed next year for a final determination of current measles elimination status, the U.S. feels that they are able to substantiate, with data, that the outbreaks that lasted close to a full year (NYC and NYS), actually ended within the required time period (most of the outbreaks ended in shorter time periods). The WHO Elimination Program does not have any expectation that occasional travel-related measles cases, and even outbreaks, will be completely prevented while cases exist in countries and areas around the world. However, it does expect, with appropriately high vaccination rates, that measles will not become endemic within a country’s borders. The United States works continually with the Pan American Health Organization (PAHO) to keep those invested in the elimination of measles internationally, informed about U.S. measles surveillance and its accompanying data. In the coming months, the CDC and the PAHO Regional Verification Commission will be reviewing U.S. data to verify and confirm that measles elimination status is warranted.
The U.S. government as a whole, public health authorities, health care practitioners, and the population of the entire country worked hard to achieve measles elimination status and to keep it. Losing it, and then achieving elimination status again, would require time and increased resources so a huge effort remains in place to prevent a loss of status. However, other than moving from the list the of not having to the list of having endemic measles, there are no real penalties for losing the elimination status nor would it jeopardize current or ongoing immunization programs or funds. Travelers from other countries or other parts of the U.S. might have recommendations for enhanced measles vaccination before traveling, or have warnings against travel, to an area in the U.S. known for endemic measles.
Resources & Links:
For information on measles from the CDC including links to communicability, signs & symptoms, incubation & period of infectiousness, complications, sequela to the disease, prevention, and more, see the CDC site: https://www.cdc.gov/measles/index.html
For CDC information on measles outbreaks in the U.S., and links to state & local health departments with outbreaks, see: https://www.cdc.gov/measles/cases-outbreaks.html
For more info about the measles elimination program with links to the WHO program and U.S. published literature on the subject, see: https://www.cdc.gov/measles/elimination.html
In late July 2019, the CDC published a new set of recommendations specifically for Healthcare Personnel (HCP) regarding measles. It should be read by anyone interested in the Prevention and Control of Measles. It’s called the CDC Interim Infection Prevention and Control Recommendations for Measles in Healthcare Settings (7/19) & contains a lot of information with many links to supportive documentation. Find it here: https://www.cdc.gov/infectioncontrol/guidelines/measles/index.html
This CDC Interim document specifically names EMS as part of the HCP group and makes reference to EMS a couple of times. Unfortunately, it leaves EMS to try and apply the recommendations by weeding out those that are applicable to EMS (and other First Responders), rather than have a specific document that acknowledges the issues particular to EMS/First Responders. So, we’ve produced a document that has been posted in an attempt to give the CDC Recommendations an EMS/First Responder spin.
This EMS-friendly version of the document will be found on this same Health Intelligence Page (HIP) under the category of Keeping Your Employees Safe and will be called EMS/First Responder Application of the CDC Measles Recommendations. It will supply specific recommendations for First Responders, particularly those providing EMS care. It also includes links found within the newly published CDC Interim Infection Prevention and Control Recommendations Guidance for Measles in Healthcare Settings (7/19) in a link found above.

